By Susan Leclair
White blood cells are so called because when you separate cells by centrifugation, they appear to be a small fluffy white cloud resting on top of the red cells. There are several ways to identify them and two different ways to count them which adds to the confusion.
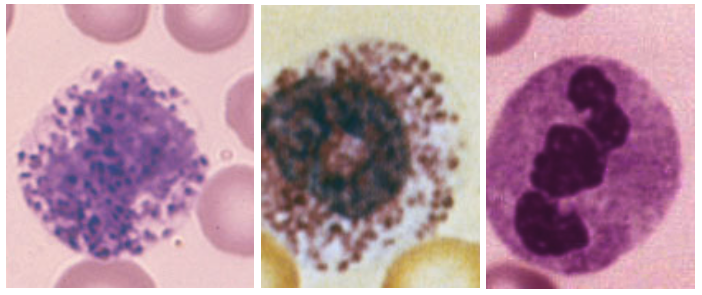
Granulocytes
This term should refer to all white blood cells that contain granules. That would mean the cells with large dark blue purple granules (basophils), cells with bright orange yellow granules (eosinophils), cells with mixed pastel (blue, pink and violet) colored granules (neutrophil) and their cousin with small sized blue and purple granules (monocyte). But, since the neutrophils are the dominant white cell seen in the peripheral blood, and monos, basos and eos can sometimes not be found in an examination of the blood, it became easy to slide into laziness and called the neutrophils (NE or NEUT granulocytes (GR or GRAN).
Of the neutrophils, you should see only two forms in the peripheral blood – the mature cell sometimes called the polymorphonuclear leukocyte (POLY or PMN) and more rarely with be called a segmented cell since the nucleus very often will have a visible segment in its nucleus and the band form in that the nucleus is not twisted or darkened. Both of these cells function identically but since the band form is slightly younger than the PMN, the distinction can be useful to determine the timing of some stress.
The younger forms of the neutrophils should be in the bone marrow and not in the peripheral blood. People with bone marrow conditions that put a lot of stress on the marrow will occasionally have some of these out in the blood as a result of that stress. Stress can also happen from any cellular damage like bruising, infection, emotional stress, and the like.
Eosinophils (eos) are the cells with the large orange yellow granules. They are most active in allergies and in responding to particular types of chemicals. Frequently they can be seen in reactions to medications. Often seen in folks with hay fever or other mild forms (unless you have them) of allergies.
Basophils are similar to eos in the sense that they are functional in allergic situations but their action is not to give you a runny nose. They act to increase blood flow into an area so that eos and the other cells can get to the offending agent. To do this they express very strong chemical that enlarge the blood vessel diameter, thus also dropping your blood pressure quickly. They also release heparin, a type of anti-coagulant, again to make it easy to get cells to move around. Finally, the changes in blood vessel diameter can cause itching which can be severe.
Monocytes are called this because their nucleus, while rather loose and free form is never segmented. Even old moby dick here has a single nucleus. This cell is the body’s trash collector. Their function is to clean up all dead, dying, damaged cells and make the area acceptable for replacement by renewal cells. They can have vacuoles (open like spaces) which result from having phagocytized (eaten and degraded) foreign material.
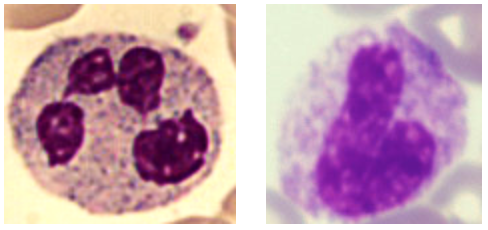
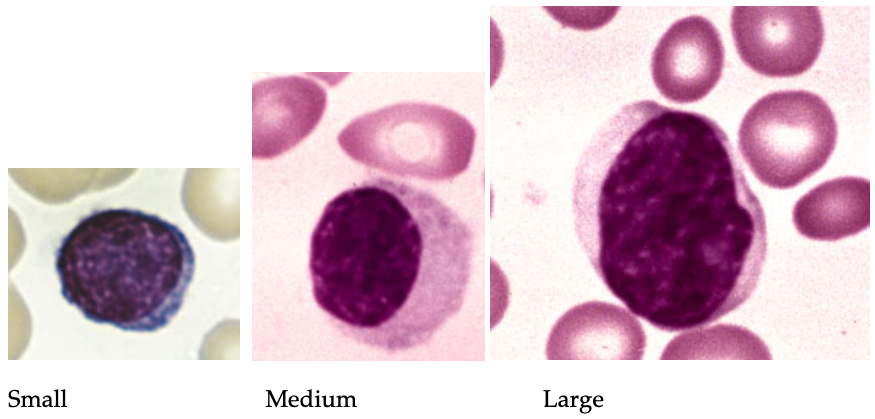
Lymphocytes come in three different sizes and are split into two major functions. The major functions were first described in chickens. One set are called T cells since they arise from the thymus gland that both humans and chickens have. The other set are called B cells since they arise in the bursa of chicken. Humans don’t have a bursa but these cells arise in the bone marrow so the B designation counts. When you look at them, it is very difficult to distinguish one from the other by function. If you look at them by size, you can guess that the larger ones are more likely T cells and the small cells are more likely B cells and the mid-sized ones are likely to be NK cells but it is that an educated guess.
T Lymphocytes
T cells are the controller of your immune system. Once a monocyte or neutrophil phagocytizes a foreign entity (cold virus, flu, bacteria, fungi, pollutant, etc.), they degrade it until it is no longer functional but still has an identification protein. This protein is transferred to the T cell which determines what type of immune response is appropriate. They then turn that response on and, when the entity has been eliminated, turn the immune system off. These are the cells that are described sometimes as surveillance cells since they should be able to recognizes and direct a targeted attack on malignancies
B Lymphocytes
B lymphocytes prefer to sit inside lymph nodes (think throat or armpit), the lymph organs (spleen, liver) and the bone marrow. These places afford a very comfortable place from which to export antibodies. The antibodies are directed by the T cells and the cells are expected to first make IgM type antibodies for the active phase of immune response and then switch to a longer lasting memory form of antibody IgG. The cells that line your GI tract and other mucus membranes (ex. Nose) will also make a third type of antibody called IgA. This stuff is simply poured into the area lined by these cells.
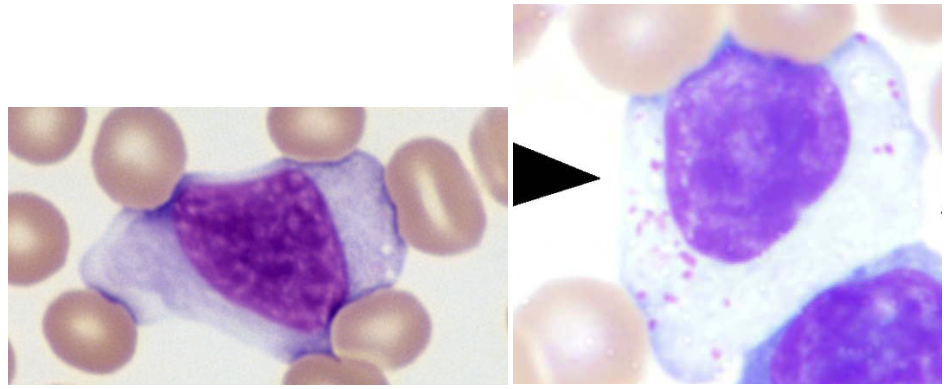
When lymphocytes recognize these foreign chemicals, they react – thus the name reactive lymphs. They tend to get larger, with much more cytoplasm, and a bigger nucleus. These are not abnormal cells. They are doing what they were made to do. In the 1920s, they were first described as “atypical” lymphocytes but that term suggests that they are damaged in some fashion. In the 1960s when the immune system was first described, they name was changed to reactive in order to reflect their health and their function.
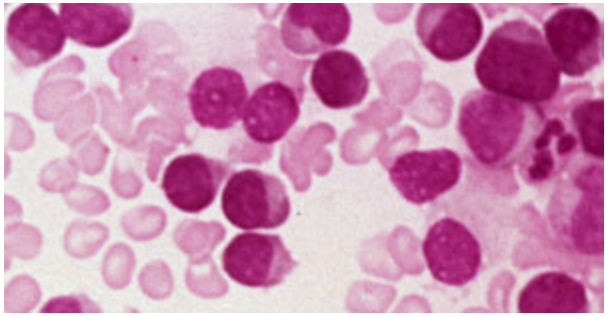
CLL CELLS
Notice that these lymphocytes are somewhat monotonous in appearance – about the same size and color and ratio of nucleus to cytoplasm. All of cells arose from one damaged cell. Since normal lymphocytes are supposed to be ready to deal with the millions of chemicals that should be dealt with, a monotonous appearance suggest that these cells will only react to one or no stimulus.
Differentials
The original differential is the percentage (%) differential. Take a drop of blood and spread it out on to a glass slide. It tends to look like a flame. Like the Goldilocks fairy tale, there is one end which is too thick and the cells stack one on top of the other, one portion that is too thin distorting the cells, and the middle section which allows you to view one cell at a time. The evaluation consists of identifying the first 100 cells you see with no skipping. The idea is that this percentage gives you a reasonable reflection of the cell population that is present. The shortcoming with percentages is that they must always total 100 so an increase in one cell type must be seen with a decrease in another cell type. For example, if your report says 90% polys and 10% lymphs, the unanswerable question is which cell is in stress? The too high polys or the too low lymphs.
The second style of differential is called the absolute (ABS or #) differential. There are two methods to arrive at these values.
- Multiply the white cell count and multiply it by the percentage of each cell. The result is the number of that specific cell within that number of white cells.
Or
- Use an instrument which will identify each cell as it passes through a counting area, thus getting both the total cell count and the actual count of each cell type.
If you take the 90% polys and 10 % lymph example, you can see the importance of knowing the absolute number.
| White cell count | %polys | %lymphs | #polys | #lymph |
| 10,000 or 10 | 80 | 20 | 8,000 H | 2,000 N |
| 100,00 or 100 | 80 | 20 | 80,000H | 20,000H |
| 3,000 or 3.0 | 80 | 20 | 2,400 N | 600 L |
Which is best? Both have their value. The percentage is easy to read and is totally adequate for the vast majority of patients, so you don’t need expensive instrumentation. The absolute differential is very clear as to the cell in stress and should be used in everyone who has some type of hematologic disorder or a hematologic consequence of some other condition.
Susan Leclair is Chancellor Professor Emerita at the University of Massachusetts Dartmouth; Senior Scientist, at Forensic DNA Associates; and Moderator and Speaker, PatientPower.info – an electronic resource for patients and health care providers.
Originally published in The CLL Tribune Q1 2019.