
By Bob Barton – Patient
Introduction:
As a treatment-naïve CLL patient, I had to make a decision on my imminent treatment. The choice was either Bendamustine-Rituximab (BR) or Ibrutinib. I was full of fear, uncertainty and doubt about the quality of life I would experience while on Ibrutinib and I found that a BR regimen would be kind of crummy but was 6 months and I would be done. My research had yielded a list of side effects but no personal perspectives on how their life may have changed.
I’m writing this article for those patients like me who are concerned about how it will affect them and their activities, and their quality of life once on Ibrutinib. Here is my experience. I hope it helps anyone who is facing treatment and needs some personal perspective to make a decision.
Background:
I am a 68 year old male and was diagnosed with CLL / SLL in August 2008. Naturally, I was placed on watch and wait. In Aug 2015, my blood work showed a rapidly increasing WBC, a dropping HGB, and I was having some episodes of fatigue. My wonderful and caring local hematologist at UMass Medical Center wanted me to start BR chemo-immunotherapy. She was also telling me I was eligible for a treatment naïve Ibrutinib trial but I was unsure of how to proceed. In general, I felt well.
I had been tracking the progress of Ibrutinib and the newer ACP-196 – now Acalabrutinib – and hoping I could join a trial. Ibrutinib trials for treatment naïve were already winding down and there was an Acalabrutinib treatment naïve trial just ending accruals.
I was fortunate to speak with Brian Koffman who encouraged me to add a CLL specialist to my team to help me with treatment decisions. Since I live 45 miles from Boston, I found Dr. Jennifer Brown at Dana Farber Cancer Institute. She was available and very willing to help.
My first visit to Dr. Brown was in October 2015 and the results of blood testing (18 vials!) showed Trisomy 12, NOTCH1, ZAP-70+, CD38+, LDH of 533, and my IGVH status showed both mutated and unmutated. My HGB was 12.2 and RBC was 4.3 and my WBC was 93,000. Although my spleen was enlarged, Dr. Brown told me that I did not meet her criteria for treatment yet which was usually signaled by HGB < 11 among other factors. I weighed 148 lbs at the time. So we watched and waited a little more.
The treatment naïve Acalabrutinib trial was closed to new patients, and my future treatment was likely going to be BR unless Ibrutinib was approved for treatment naïve CLL. Another Acalabrutinib trial was opening with 3 arms so I had a one in 3 chance of getting chlorambucil or Obinutuzimab + Acalabrutinib or Acalabrutinib. Unfortunately, the closest trial center was several hours drive away and I couldn’t be certain which arm I would be in or if I could drive to and from the treatment center. I had to abandon that idea unless the trial started in Boston. As of this writing, it still has not started.
Several more visits to UMass showed my WBC rising rapidly to 125,000 and HCT dropping below 11. In February of 2016, both my local hematologist and Dr. Brown told me that Ibrutinib may be approved soon for treatment naïve CLL. .I started researching all the side effects and quality of life of patients on Ibrutinib but this wonder drug seems to affect people differently and I could not correlate any data with my specific CLL markers.
In late February I experienced the worst bout of fatigue ever. It lasted for several days and my skin color was gray and I could barely make it through the day and I did not want to get up out of my chair. I was concerned that I needed to start treatment right away and still was not comfortable with BR treatment. I was also aware that my first grandson would be born in 2 months and my middle daughter would be getting married in 5 months. I did not want to be ‘chemo-impaired’ for either of those two events. The timing was bad for me to be heading into BR chemo-immuno therapy treatment.
My constant research revealed that there was a trial of Curcumin starting for CLL. Unfortunately it was given with another drug that I couldn’t take. But the research article said Curcumin inhibits pro-survival pathways in B-CLL so I bought 500mg capsules of High Absorption Curcumin and started taking one per day in the last week of February.
In early March, Ibrutinib was approved for treatment naïve CLL. I checked Dana Farber for the Acalabrutinib trial, but it would be several more months before it would start. It looks like Ibrutinib was going to be my salvation but I couldn’t be sure of the adverse effects and wished someone wrote an article on the quality of life one could expect while taking Ibrutinib. I was concerned about how soon diarrhea would start, the severity, bruising – because my work often gets physical. I was worried about atrial fibrillation because I wanted to get back to my regular workouts that I neglected due to fatigue. I lost muscle mass in the previous 6 months and I wanted it back. I worried about what time of day I should take it – with food or without. I really worried if it would affect my being there for my grandson’s birth or my daughter’s wedding.
I did more research and found that there were no guidelines for taking it with food because testing showed no evidence of any difference when taking Ibrutinib before, during or after meals. I researched if there were any precautions to be taken regarding sexual relations. The only thing I found was regarding pregnancy and to use birth control. I found out that Ibrutinib isn’t poisonous like chemotherapy drugs meaning your partner won’t be poisoned with toxic chemicals from saliva and other body fluids. Caution is always recommended and to be safe, condoms can be used to limit bodily fluid exchanges.
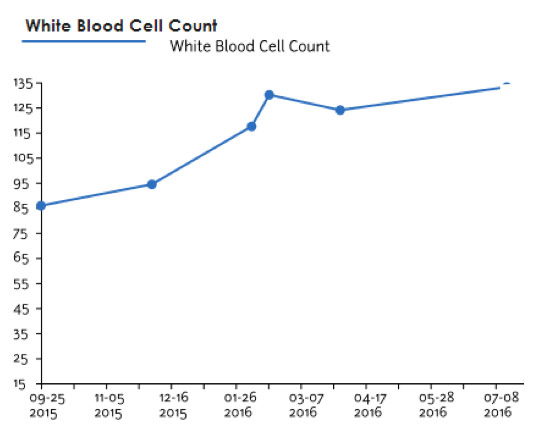 Since I started the Curcumin, I felt nearly normal but often tired in the afternoons. My WBC levels seemed to stabilize at 130,000 but I was losing weight while I held off starting treatment. My local hematologist and I agreed that I would start Ibrutinib mid-July after my daughter’s wedding. So we prepared by scheduling the CT scan in June and the bone marrow biopsy in July.
Since I started the Curcumin, I felt nearly normal but often tired in the afternoons. My WBC levels seemed to stabilize at 130,000 but I was losing weight while I held off starting treatment. My local hematologist and I agreed that I would start Ibrutinib mid-July after my daughter’s wedding. So we prepared by scheduling the CT scan in June and the bone marrow biopsy in July.
That was the second bone marrow biopsy that I had had and still I was amazed at how little pain was involved. My hematologist did both of them and she did them really well.
Once the prep was done, it was time for treatment and I felt like I was going through a one-way door into a lifetime of treatment on Ibrutinib. I had serious doubts that I should do this. My hematologist, Dr. Brown and Brian Koffman reassured me that I would be fine on Ibrutinib. Why was I not convinced?
Starting Ibrutinib – The First 30 days
Before starting Ibrutinib treatment, I was 138 lbs, my WBC was 133,000, RBC was 3.54, HGB was 10.4 and my LDH was 733! My blood pressure was 112/71. My spleen was massively enlarged at 23.5 cm which is slightly more than double in size from the normal 11 cm. And while my liver felt larger, the CT scan showed it was normal. My lymph nodes in my groin were like big clusters of grapes and under my arms were large fleshy lumps easily seen and felt. My gut was distended to the point that my belly button herniated and you could feel my spleen near the mid-line of my abdomen. My hematologist prescribed Allopurinol which is a uric acid reducer to help alleviate any effects of the breakdown of my large tumor load.
Saturday July 16 was going to be my start day, but I decided to take the Allopurinol first to see if there were any side effects. Some of the listed side effects were fever, sore throat, blood in urine and I did not want to confuse side effects with Ibrutinib. The Allopurinol had no side effects for me that first day.
Sunday July 17th was Day 1 that I took my 3 capsules of Ibrutinib before breakfast with water. I then made myself a cup of coffee and continued my day. The day was uneventful. I was drinking more water and therefore urinating often, but no adverse effects. I took the Curcumin during dinner and Allopurinol after dinner.
I followed the same routine for the next two days. I was drinking about two liters of water more than I normally did. I eat at least 3 meals a day plus some snacks. I’m trying to gain some weight. All was good.
By Tuesday Day 3, I imagine that my armpit nodes are smaller. Could that be true? They feel smaller but like I said, it could be my imagination. Later in the day my intestines are rumbling and by mid afternoon I have my first loose stool bowel movement. It could have been the beginning of full blown diarrhea, but things settled. I had another small loose stool near bedtime and that was it.
Day 4 I feel a little rumbling but it diminishes. I weigh 139.5 lbs. No side effects and I keep to my routine of Ibrutinib first thing in the morning on an empty stomach, then coffee, then breakfast, a snack of nuts, lunch, dinner, Curcumin, and Allopurinol.
Day 5 brings noticeable reduced groin lymph nodes and underarm nodes definitely feel smaller. I run out for an errand, mow the lawn and I notice that I still have some energy. I feel ok. It’s hard to say if I feel better than before starting Ibrutinib because I often feel ok since starting the Curcumin.
I’m supplementing my food intake with either Boost or Ensure brands of protein shakes – especially if I get too busy and miss lunch. Lunch is either 2 eggs and toast, or turkey or tuna salad sandwich on a hard roll. Sometimes I’ll eat oatmeal. I continue drinking a lot of water during the day.
Saturday, Day 7 is Pancake Day at my house. I eat a short stack before driving to my daughter’s house an hour away. The day is unremarkable otherwise.
So after 1 week on Ibrutinib, I feel lucky about having minimal side effects. I weigh 140 lbs and my bowel movements are normal.
The next two days are unremarkable but on Tuesday I’m working on my feet all day doing some body rust repair on my car. I’m definitely tired by dinner. All I want to do is relax. The next day, I work on my car again. This is Wednesday, Day 11 and I feel so fatigued by 5:00 PM that it reminds me of last February’s melt down. After dinner I drop off to sleep for a short nap then get up and go to bed earlier than usual.
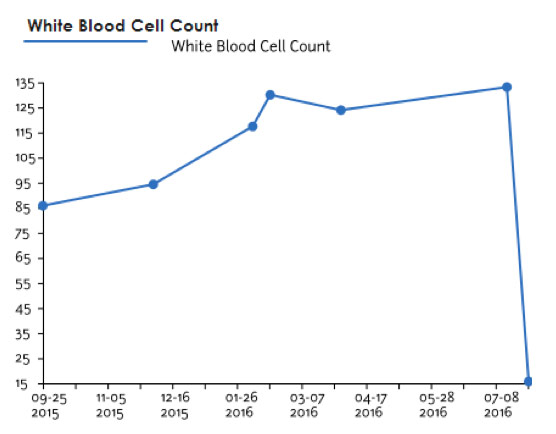 By Day 13, I weigh 142.5 lbs and I am due for a checkup at UMass. My blood counts show dramatic drop in WBC from 133,000 to 15,000, HGB inched up to 11 and platelets dropped to 84 from 127. My LDH went from 733 to 127! Spleen seems to be shrinking along with lymph nodes.
By Day 13, I weigh 142.5 lbs and I am due for a checkup at UMass. My blood counts show dramatic drop in WBC from 133,000 to 15,000, HGB inched up to 11 and platelets dropped to 84 from 127. My LDH went from 733 to 127! Spleen seems to be shrinking along with lymph nodes.
Day 14 is unremarkable except for late afternoon when sitting. I notice my heartbeat is heavy, or thudding, in my body. It’s not fast. I’ve had this feeling before so I’m not too concerned. Days 15 and 16 are unremarkable.
Day 17 I notice pain in my chest that feels like heartburn or acid reflux pain. It came on 5 minutes after eating a cherry tomato off the vine. Heartburn appears to be one of the side effects of Ibrutinib. My weight is somewhat stable at 143 lbs, give or take a pound each day.
Day 18 is a weight training day. I used to do strength training 2 days a week but I was running out of breath for the past 3 months and stopped. Today feels like I am improving enough to tire my muscles before I get tired. I’m happy about that. The heartburn continues especially at bedtime but lasts only about 10-20 minutes. I also notice it occurs when I bend over doing something like picking up tools or getting laundry out of the dryer.
Day 20 – I walk a strenuous mile up steep hills like I was doing last year. Day 21 and 22 are weekend days where I have no schedule except for my Ibrutinib pills. Sunday is a round trip drive to NJ for my grandson’s baptism celebration with a total of 8 hours in the car. The trip was unremarkable. Day 23 is a day off just to relax a little.
Day 24 is weight training. It seems to be getting easier so I increase my weights. The next day I take a long morning walk and actually run for ¼ mile. It was tiring but in a good way as I haven’t done that since last year and my leg muscles were feeling it.
Day 26 was weight training again and I definitely feel stronger. I’m doing more reps with the heavier weights. I also notice that I don’t feel my heart beating in my ears or body like I was 2 weeks ago. I weigh 144 lbs.
Day 27 was my 4 week blood test day. While I’m there, I pick up my Ibrutinib refill. I have a few more errands to do until late day having a sausage and mushroom pizza for dinner. I don’t know if it’s a good idea since I’ve had mild indigestion all day even after eating lunch. I bought some antacids just in case but I had no heartburn after the pizza and salad. This was unexpected but worth the risk.
Day 28 is a Saturday. Sill no results from my blood work the day before but breakfast pancakes were a great start to the day. I’m looking for a way to determine if I’m gaining any muscle mass without immersing myself in a calibrated tank of water…
I am noticing vision issues in my one good eye over the past few days. I am monocular – completely blind in my right eye so I’ve been having many visits to my ophthalmologist each year for many years checking my glaucoma. Three months ago he mentioned that I had a small cataract starting in my good eye. Today I am noticing a high sensitivity to brightness like sunny areas or computer screen. I notice that my contrast vision has deteriorated. I have an appointment in two weeks but I’m going to call Monday and move it up. I’ve read papers on the occurrence of cataracts while on Ibrutinib, but evidence of occurrence seems to be the same as the normal age related occurrence common in older people.
Day 29 and the only thing on my mind is having a cataract in my only seeing eye. I still have some episodes of heartburn but again they are short lived or just mild annoyances.
Day 30 and I take the last 3 pills of Ibrutinib in the first bottle. I do have my refill ready for tomorrow’s dose. I go for my morning walk and find myself running during the second half of it without getting tired! I’m out of breath and my legs are a bit rubbery but it’s primarily because I haven’t run in a year or more. I’m pleased.
But, I am so concerned with my vision that I call my eye doctor to see him today. I also scour the internet for a connection of Ibrutinib and photosensitivity and I can’t find one. The eye doctor I see (not my usual one) can’t find anything different in my eye since my last appointment. My cataract is still small and my color sensitivity is ok plus my visual acuity is the same according to the eye chart.
I called the Imbruvica patient help line (find it at Imbruvica.com) and they have no documented cases of ocular photosensitivity on file. So, for the purposes of this article on the quality of life while starting Ibrutinib, there is no reason to go into the details of my photosensitivity.
Thirty days, one bottle of Ibrutinib later and I am feeling pretty well. My experience with Ibrutinib has been much better than I dared to hope before I started. My expectations of adverse side effects were overblown. I realize that adverse effects can show up at any time but I’m very pleased with the first month.
The next 11 days are pretty much the same. My vision is the only issue and I obsess about it and can’t wait until I see my eye doctor in a few days. I call him to move up my appointment, but he prescribes prednisolone drops and keeps my original appointment.
I see my hematologist for my blood work and 6-week checkup. My WBC has risen from 11.2 to 12.3 which doesn’t concern me because I expected my WBC to get higher when I first started Ibrutinib. My RBC is improved from 3.8 to 4.2 and my hemoglobin has gone up from 11.9 to 12.9 – a whole point! I can understand why I am less tired now.
Day 44 on Ibrutinib and I see my eye doctor and he diagnosis “Corneal Epithelium Sloughing” (CES) where the outermost cells of my cornea are shedding. This causes blurry vision and photosensitivity because of the diffraction of light changes. My eye doctor knows of Ibrutinib but nothing of the side effects. I tell him that “blurry vision’ is a reported side effect but I don’t know much about the specifics. The prednisolone raised my eye pressure so he puts me on Lotemax gel drops – a different steroid that does not raise pressure.
I’m researching for any reported causes of “blurry vision” from Ibrutinib and I call the Imbruvica patient help line again. I let them know what my eye doctor found and ask if it matches what others reported for adverse effects. They tell me that they only collect the reports of side effects and have no data to give on details of “blurry vision” reports. My CLL expert tells me that CES may well be in the realm of Ibrutinib side effects but there are no published papers with details of the blurry vision cause. I hope it resolves on its own or under the care of my eye doctor who I see again in 3 weeks. My further attempts to find details are futile so I have to wait. As I mentioned, I’ve been blind in one eye for 60 years or so, and my ever present nightmare is that I might lose my good eye one day. So maybe I’m being overly obsessive about it. I’ll wait.
Day 51 on Ibrutinib and I weigh 147 lbs and feel well enough to tackle most everyday projects and carry on with a normal 5 day workout routine.
Except for my eye issue, Ibrutinib treatment has been an easy path to follow and I’m grateful for my progress and the demise of my CLL tumor burden. I started taking Acyclovir to help ward off any attempt by the shingles virus to reactivate. I don’t know for how long I must take it, but better safe than sorry.
I hope this article helps anyone who is wrestling with the decision to start treatment. Now that Ibrutinib is available for treatment-naïve CLL patients, I would recommend Ibrutinib over chemo-immuno therapy such as BR for us older folks. In a nutshell, it’s easier.
My long term strategy is not to take Ibrutinib for my CLL for the rest of my life but to manage its progression until something better comes along. In the first month my blood counts are improved close to normal, and my lymph nodes and spleen are close to their normal sizes. Given the rate of discovery in new treatments for CLL, I am optimistic that my strategy will work out. If it does, Ibrutinib will not be a drug I have to take for the rest of my life.
I consider myself fortunate so far to have what feels like a normal life with few side effects while on Ibrutinib. Taking 3 capsules each morning is easy since I normally take my vitamins first thing in the morning. I hope your experience goes as well as mine.
Bob is a computer technologist having joined the computer industry in 1978 solving mission critical hardware and software computer failures worldwide. He designed and developed computer system solutions and products. In 2000, Bob was a founding member of a high tech startup that made high speed network switches. As Director of Engineering Operations, he was responsible for facilities management, engineering labs and equipment, Information Technology, Quality Assurance, Customer Support, and product release activities.
In 2003, Bob started his own product design company where he developed and patented the first generation of PowerSURE® Power Failure Safety Lighting wiring devices. Five years later he founded the former PowerSURE Corporation to successfully license his patents and to design additional new products.
Bob holds several patents and has helped others in their intellectual property pursuits. Bob also lectures on product development and marketing at a local technical university. He is currently experimenting with 3D scanning and printing looking for new product and service ideas.
Originally published in The CLL Tribune Q3 2016.

















