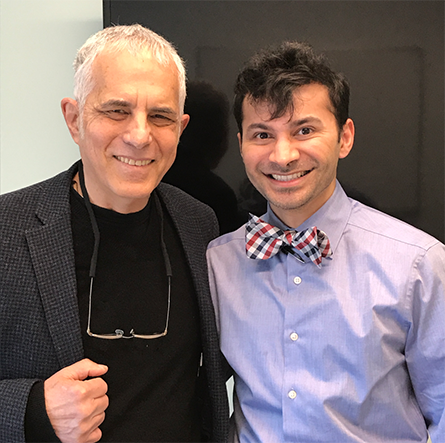
I want to introduce a remarkable young physician who you will be hearing more from in the future.
Dr. Utkarsh H. Acharya, DO, FACP is now the Program Director, Hematology-Oncology Fellowship Program, DFCI (Dana Farber Cancer Institute)/SEMC(St Elizabeth’s Medical Center) and an Attending Physician, Hematologic Malignancies, Dana Farber Cancer Institute and an Attending Physician, Cellular Therapy, Brigham & Women’s Hospital.
Everyone calls him Utty.
I knew him as my attending physician for most of my critical inpatient and outpatient care during my CAR-T trial at the S.C.C.A. (Seattle Cancer Care Alliance)/Hutch.
Utty was the one who lead the multi-disciplinary team that saw me through my darkest days in Seattle. He was a tremendous source of comfort for Patty, our daughters and me when things looked bleak; a beacon of medical knowledge, a responsive, compassionate physician, and a fountain of patience when dealing with a doctor as his patient.
I am forever grateful for his kind and skillful care.
Soon after I headed home from Seattle after my time as a patient and trial subject, he also left, in his case, for Harvard in Boston.
Utty prefers to write thoughtful answers for an interview rather than talk on the fly in front of a video camera, so I will be sharing our Q & A about CAR-T and other immune and cellular therapies over the next few weeks.
Here is the first of my seven questions:
Q: Why did you personally decide to get involved in immunotherapy?
A: To me, the mere presence of cancer implies either the failure of our immune system or evasion to the immune system by the tumor. When considering systemic treatment approaches in patients with widespread disease (regardless of the tumor type), chemotherapy has been heavily utilized for the better portion of the field’s existence. While chemotherapy can be effective and certainly will continue to have a role in the management of cancer, it can be non-specifically toxic and its effects aren’t always durable or curative despite the potential to induce disease response in various disease states (i.e. CLL). It is especially less effective in the salvage settings after patients have failed or relapsed after prior inductions. Thus, new modalities of treating cancer are necessary in cases of chemotherapy failure. Fortunately, molecular profiling has advanced over the years allowing for not only prognostication of various cancers but, just as importantly, the development of targeted agents by small molecules to address cancer (i.e. ibrutinib / venetoclax). Unfortunately, however, these agents are not curative and require indefinite administration of the drug until it loses its beneficial effects. This ultimately leads us into the modern day era of immuno-oncology/immunotherapy. While present day immunotherapy is growing in terms of sophistication with the inception of novel checkpoint inhibitors and adoptive cellular therapies (i.e. CAR-T cells) to the bedside, the concept of harnessing the immune system to combat cancer is not new. Immune based treatments have been historically used in conventionally incurable conditions such as metastatic melanoma and renal cell carcinoma with high dose IL-2 (a potent cytokine that is known to populate T-cells – our body’s own natural cancer killing cells) with the potential to induce long term remissions in select patients. Additionally, allogeneic hematopoetic stem cell transplant is an immunotherapeutic modality, which has the potential to induce cures through a “graft versus tumor” effect as demonstrated in patients with aggressive blood cancers with high risk disease or were incurable by chemotherapy. Thus, the present day approach of harnessing and engineering the immune system through CAR-T cell therapy was of personal clinical interest as an oncologist.

















