By Susan Leclair
First starting from a stem cell that is only found in the bone marrow, one can think of platelets as the broken off pieces of cytoplasm of the cell megakaryocyte. The megakaryocyte is, as its name implies, a large stem cell with what is usually described as abundant cytoplasm. All platelets come from megakaryocytes in the marrow. Once broken off into these smaller pieces, the platelet or as they are sometimes called, thrombocytes, rearranges the compounds and structures within itself. Try to think of a platelet as a high-grade sponge with various sized blind holes that can be both shallow and deep. The resting platelet tends to look like a fully saturated sponge – round and slightly puffy.

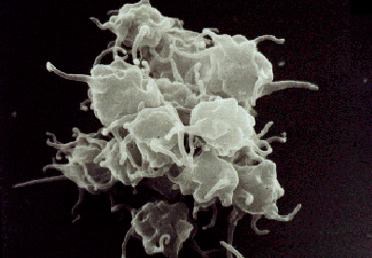
Inside those pores and recesses, coagulation proteins and other compounds collect so when the platelet is activated, the sponge can get squeezed and the internal material of the platelet can interact with the externally collected fluids to form first a mesh and then, once entangled with the fibrin, a blood clot.
Platelet counts
The traditional method of counting platelets was terribly time consuming and required additional equipment so it was not considered part of the CBC until the 1980s when automation started to help out. The older method counted (somewhat imprecisely) platelets. The instruments count any particle that is of a certain size range so very small red cells, pieces of white cells, etc. can falsely increase the count. Very large platelets are usually counted as red cells, forcing the platelet count to appear to decrease.
Thus the reproducible range of repeated platelet counts on the same specimen is much wider than wished.
Another potential problem with the platelet count is that they can clump together in the bloodstream and not be counted by the automated machines leading to a falsely low count. Some hematologists will use an old school light microscope to exam the blood when there is thrombocytopenia (low platelets) to confirm if it is real and not due to clumping.
The other issue with the platelet count is one seen with red and white cells. Nothing tells you of their function. The anticoagulant used in the test tube in which a specimen is drawn renders the platelets inactive so you can’t tell what they are doing. They are so small that the internal construct of the platelet cannot be seen well so it is hard to make comments about their granules (should be there) or vacuoles (shouldn’t be there), etc.
There are several causes for low platelets
- Bone marrow crowding or damage from cancers, drugs or other diseases where there are inadequate precursor megakaryocytes
- Destruction of the platelets in the blood stream by an auto-immune process called ITP (Immune thrombocytopenic purpura)
- An enlarged spleen that captures (sequesters) too many platelets
Too few platelets can commonly lead to increased bruising or bleeding into the skin (large bruises are called ecchymoses, small ones are petachaie), and in worse cases serious internal bleeding.
Platelet Function Tests
The short answer here is that there are not many and those have a tendency to be available in large facilities only. Platelets can be tested to see if they respond to chemicals that should cause them to clump together. This means we can comment about both inherited and acquired von Willebrand’s Disease, aspirin, clopidogrel, and prasugrel medication, and some rare inherited disorders. There are no good tests to discern the various stages of platelet function (activation, aggregation, retraction) since all of the biochemical activity is occurring at a level that would require electron microscopes. Unfortunately, electron microscopy usually requires a dead, fixed bunch of cells so that interaction cannot be seen.
Susan Leclair is Chancellor Professor Emerita at the University of Massachusetts Dartmouth; Senior Scientist, at Forensic DNA Associates; and Moderator and Speaker, PatientPower.info – an electronic resource for patients and health care providers.
Originally published in The CLL Tribune Q4 2018.


















