Targeted therapies are very effective and have become the standard of care for treating chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL). While chemotherapy broadly kills rapidly dividing cells, targeted therapies are drugs or other substances that target specific enzymes, proteins, or other molecules involved in the growth and spread of cancer cells. Two widely used classes of targeted therapies are covalent Bruton tyrosine kinase (BTK) inhibitors (i.e., ibrutinib or acalabrutinib) and BCL2 inhibitors (i.e., venetoclax). While these therapies have led to improved outcomes and durable remissions for many patients, a subset of patients will have their CLL / SLL progress after treatment with these agents. So what treatment should come next after patients have already been exposed to the major targeted therapies currently in use? Currently, there is no clear answer or standard of care, but researchers are trying to learn more.
At the annual meeting of the American Society of Hematology (ASH) 2021, Dr. Anthony Mato, Director of the CLL program at Memorial Sloan Kettering Cancer Center in New York, interviewed Dr. Megan Thompson, a Medical Oncology/Hematology fellow at Memorial Sloan Kettering Cancer Center. They discussed results from two new studies, which looked at real-world outcomes of subsequent therapies in patients whose disease progressed after either 1) double-exposure to a covalent BTK inhibitor and venetoclax or 2) exposure to a non-covalent BTK inhibitor.
Takeaways From Study #1:
- The BTK inhibitors ibrutinib, acalabrutinib, and the BCL2 inhibitor venetoclax are the primarily targeted therapies that are standard care for most CLL / SLL patients.
- In the clinic, doctors are now seeing some patients whose disease has progressed after having been “double-exposed” to a BTK inhibitor and venetoclax.
- Since this is an emerging issue, not much is known about the best course of action.
- Researchers wanted to find out how clinicians treated “double-exposed” patients in their practices and what outcomes patients were experiencing.
- For this retrospective study, 125 patients were identified that had previously been treated with both a covalent BTK inhibitor and venetoclax and who had then required further treatment.
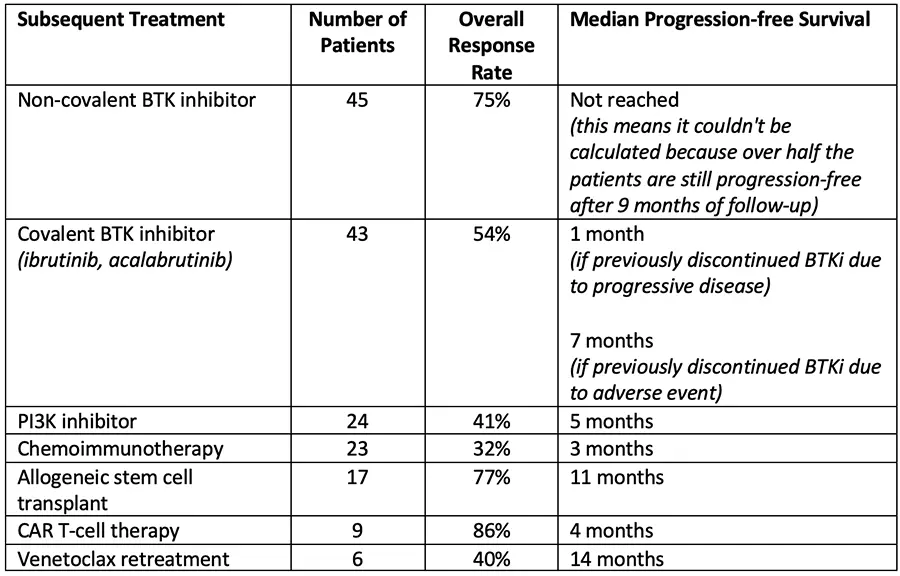
- Common treatment strategies and their corresponding outcomes are listed in the table below. More detailed information is available in the abstract.
- Non-covalent BTK inhibitors such as pirtobrutinib bind to the BTK protein differently than traditional covalent BTK inhibitors to overcome resistance mutations.
- Non-covalent BTK inhibitors are still experimental, but they produced a high overall response rate and durable responses in this study.
- Allogeneic stem cell transplant appears to be promising for select patients who qualify.
- CAR T-cell therapy produced high response rates, but due to the limited number of patients in this study, it would need further exploration.
- Even though chemoimmunotherapy and PI3K inhibitors are approved therapies, they had poor outcomes and responses that were not durable in this context.
Takeaways from Study #2:
- Non-covalent BTK inhibitors are still experimental and are in clinical development for treating chronic lymphocytic leukemia (CLL) and Richter transformation.
- These agents (pirtobrutinib (formerly LOXO-305), nemtabrutinib (formerly ARQ 531), vecabrutinib (formerly SNS-062 but no longer in development) reversibly bind BTK and overcome acquired resistance to covalent BTK inhibitors.
- Researchers wanted to find out how clinicians treated patients who progressed after treatment with a non-covalent BTK inhibitor and what outcomes patients were experiencing.
- For this study, 42 patients with CLL or Richter transformation were identified who were treated with and subsequently discontinued a non-covalent BTK inhibitor.
- Of these patients, 32 (76%) received another line of therapy.
- Because the number of patients is so small, this data is more for hypothesis-generating rather than drawing any definitive conclusions.
- CAR T-cell therapy was promising, with good overall response rates (ORR = 80%).
- Venetoclax was helpful if the patient had not previously been treated with it (ORR = 60%).
- Chemoimmunotherapy produced poor outcomes in both CLL (ORR = 33%) and Richter transformation (ORR = 13%).
Conclusions:
One of the evolving questions in CLL / SLL management is what sequence should all these different therapies be given in? For example, Chemoimmunotherapy used to be a standard first-line treatment, but that is no longer the case, and it is used in a much more limited fashion. Now targeted therapies such as ibrutinib, acalabrutinib, and venetoclax are standard first-line therapies that offer better patient outcomes. However, these therapies are not curative, so some patients will eventually progress, and clinicians must figure out what subsequent treatments should be used. These studies offer a glimpse into the future of what will likely become increasingly common scenarios for clinicians. Hopefully, as this data continues to be updated, it can help guide clinicians on what treatment strategies might be helpful for their patients.
Outside of clinical trials, there are essentially only two classes of drugs to treat CLL / SLL: a BTK Inhibitor (ibrutinib, acalabrutinib, and off-label use of zanubrutinib) or the only approved BCL-2 inhibitor, venetoclax. Both can be used with and without monoclonal antibodies (rituximab and obinutuzumab) to improve responses. Once these medications fail patients, their options are limited, and their prognosis is challenging. These “double-exposed” or “double refractory” patients where both classes of medication are no longer effective have one of the most significant and fast-growing unmet needs in CLL / SLL
Please enjoy this interview with Dr. Thompson from the ASH meeting, held in December 2021 in Atlanta, GA, and virtually.
You can read the actual abstracts here:
Take care of yourself first.
Ann Liu, PhD

















