It’s been a while since our last COVID-19 Update in May when the end of the public health emergency was declared, resulting in a severe lack of funding for tracking the disease metrics. US COVID-19 infections are hovering near levels of the pandemic’s first peak in 2020, and approaching the Delta peak of late 2021, according to wastewater surveillance.
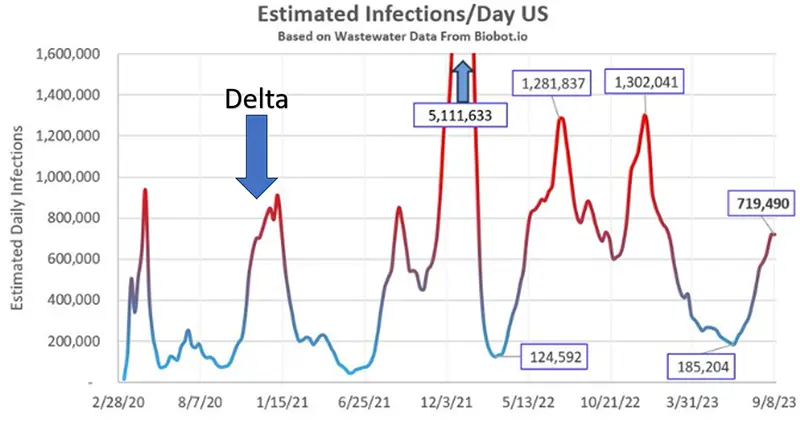
Based on US wastewater data (which is our most accurate indicator right now), it is estimated that there are currently:
- 720,000 new infections/day nationwide
- 1 in every 460 new people were infected today
- 1 in every 46 people are currently infected
It is predicted that an additional 7-10% of the US population will become infected with COVID-19 over the next six weeks from this surge. Biobot data models show cases are beginning to slightly recede, but it is predicted they will plateau and then surge to even higher rates in late fall and winter. It’s yet another sign that while the government’s state of emergency declaration may be over, COVID-19 is far from over. Since we are once again experiencing a surge in COVID-19 cases, a rise in hospitalizations, and a rise in deaths, we wanted to provide our community with a snapshot of where we currently stand at this point in the pandemic.
Keep in mind that since the end of the public health emergency on May 11, 2023, the data points that were previously crucial to accurately understand and assess our own personal risk in the communities we live in is no longer consistently reported by government sources, if at all. And when it is reported, the data points that we are able to obtain are heavily delayed-sometimes by weeks.
Weekly COVID-19 Statistics
The COVID-19 Wastewater Monitoring Project, last updated September 13th, paints the most accurate picture we can have of true case numbers, as wastewater levels are not dependent upon people testing or health departments being required to report data. Note the top dark blue line (which is the amount of coronavirus measured in wastewater) indicates we are currently in a surge that has slightly receded.

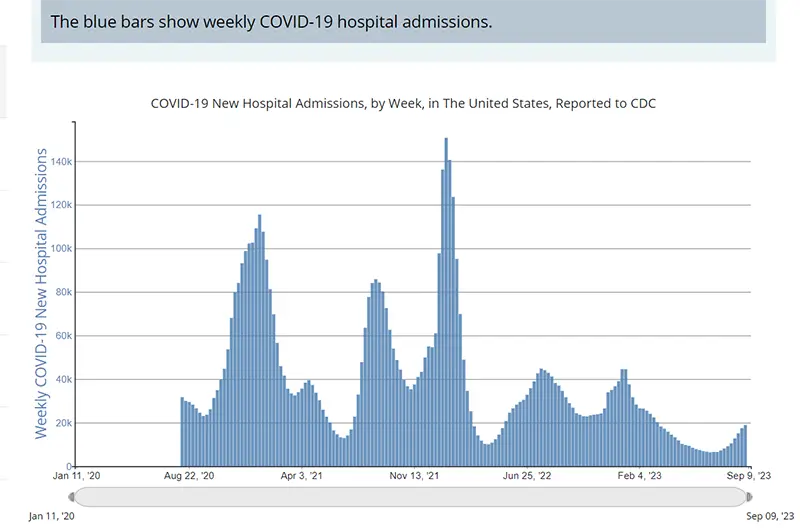
The rate of hospitalizations, last updated on September 9th by the CDC, indicated an increase in the number of individuals hospitalized for COVID-19.
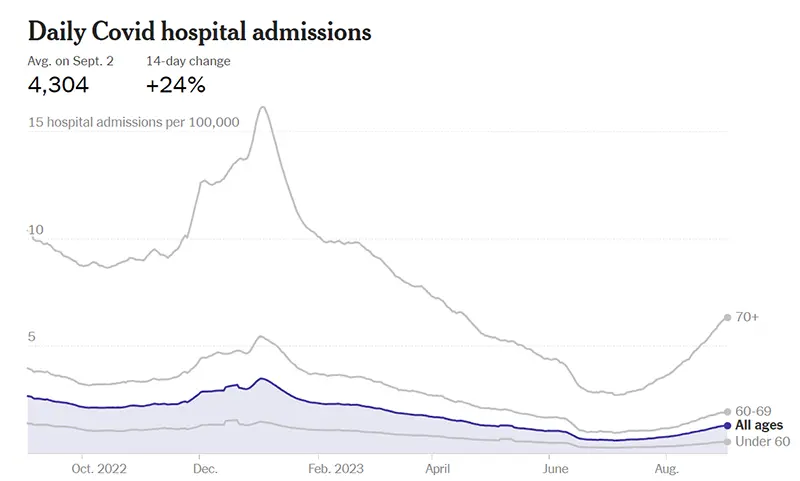
Here is a screenshot from the New York Times of hospitalizations, last updated September 1st, broken down by age groups. As has consistently been the case throughout the pandemic, those above the age of 70 are at much higher risk of hospitalization for severe COVID-19 disease.
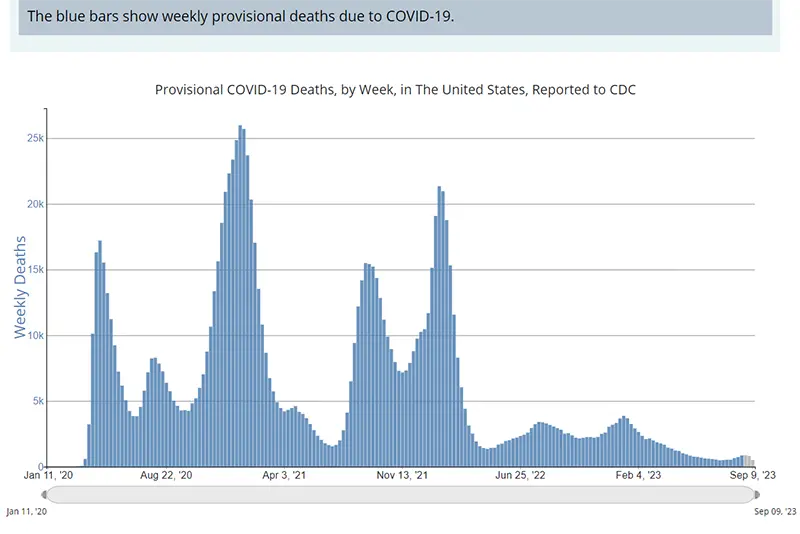
The weekly average number of COVID-19 deaths in the US ending the week of August 18th was 860 (this is one of the data points that is heavily delayed). Reported numbers of deaths are a lagging indicator, especially now that timely reporting of numbers is no longer required by the federal government.
Current & Emerging Variants of Concern (VOC)
Here is the overall breakdown of variants in the US according to the CDC’s Variant Tracker as of September 16th. If you have been following these weekly updates, you will notice there is no longer a dominant variant, but rather MULTIPLE variants that are all competing for dominance.
The ability to follow which variants are out there has become even more confusing and difficult to follow as of late with this new variant soup (as some are calling it). We are in a phase of the pandemic where there are so many nearly equal circulating variants, with no one variant taking over complete control. However, it is important to know that there are three “variants of interest” and there are seven “variants under monitoring” that the World Health Organization (WHO) is monitoring around the world. The two variants currently driving the surge in the US are EG.5 and FL1.5.1.
Here’s a summary of what we know:
EG.5 This variant is also referred to as the Eris variant and is currently a “variant of interest” according to WHO. Right now, it equates to about 25% of the variants being sequenced in the US. It is a sub-lineage of Omicron and it has an increased growth advantage, meaning it can transmit extremely efficiently from one person to another. We are seeing waves of infections due to EG.5, meaning it is beginning to slightly outcompete some of the other variants that are in circulation. We are not seeing a change in the severity of infections due to EG.5, although it can still result in severe disease and death.
FL.1.5.1 This variant is referred to as the Fornax variant and is currently responsible for around 14% of cases sequenced in the US. It is a descendant of XBB, and it has a mutation in it that helps to increase its contagiousness. The cases of Fornax have been nearly doubling every week. This variant is derived from XBB.1.9.1, and Moderna has reported that their newly updated vaccine neutralized this variant in the human clinical trials.
BA.2.86 This variant is also referred to as the Pirola variant and the WHO recently classified this one as a “variant under monitoring.” The reason for this is that there are 36 new mutations relative to XBB.1.5, with 30 mutations located on the spike protein and several key mutations located on the receptor-binding domain (that are not located on the spike protein). It is those mutations located on the receptor-binding domain that are concerning due to the higher likelihood that the variant can have some immune escape against our newly updated vaccine and any past immunity acquired from natural infections. So far there are very few cases that have been detected only in Michigan, Virginia, and Ohio. However, it has been detected in wastewater around the world. Right now, we have very little information to assess the effects of this variant, but researchers are watching this one very intensely. So far, this variant is not outcompeting any of the other variants, and this is what we will be looking out for.
The newly updated monovalent vaccine will be effective against EG.5 and FL.1.5.1 since they are close descendants of the XBB.1.5 variant for which the new COVID-19 vaccine was updated against. But if BA.2.86 becomes dominant in the US, it is suspected that the newly updated vaccine may not be as protective against this variant (although it will still provide some). As has been since the beginning of the pandemic, it is good to keep an eye out for what might come. But that being said, the only thing we can truly focus on is what’s happening in the here and now. While BA.2.86 is one to watch, it’s not one to be concerned about just yet.
COVID-19 in the News
- All Americans ages 6 months and older are eligible to receive an updated COVID-19 booster tailored to the XBB Omicron strain, the CDC announced last week. The formula for the new vaccines is highly similar to the EG.5-related variants circulating in the US right now. Vaccination remains the best protection against hospitalization and death and studies have shown it reduces your chance of suffering the effects of Long-COVID, also known as post-acute sequelae SARS-CoV-2 infection (PASC). If you have not received a COVID-19 vaccine in the past 2 months, consider getting an updated COVID-19 vaccine to protect yourself this fall and winter.
Please remember, we now know there is more to immunity than just antibody levels. If you didn’t have a robust antibody response to prior doses of the COVID-19 vaccine that does not necessarily mean that you should not get vaccinated. The other, often-forgotten half of the immune system, T cells, provides protection against severe disease. There are no laboratory tests available to the public that measure T cell responses to the COVID-19 vaccine. While T cells can’t prevent infection like B cells can (and B cells are impaired in those with CLL / SLL due to them being cancerous), T cells can still help to soften the blow of a COVID-19 infection. Also, we have studies now that indicate repeated vaccination in those with blood cancers can increase one’s ability to prevent COVID-19 infection, particularly after four doses.
Mask up, wash your hands, increase ventilation when you can, get your booster, and have your COVID-19 Action Plan handy. Keeping up to date with the most recent set of vaccine recommendations for the immunocompromised, in addition to early diagnosis (test early and often), and quick access to care (Paxlovid within five days of symptom onset) can prevent severe disease and death in those with CLL / SLL.
Keep learning, and please stay well.
Robyn Brumble, MSN, RN
Director of Scientific Affairs & Research
CLL Society

















