
By Erin Michaela Sweeney – Patient
It was so emotionally painful to be apart from my baby boy, but I gained wisdom with my time of heartache. During my time in isolation away from Eliott, I longed to stroke his hair, look into his eyes, feel his warm hug. I was fearful that I would miss an important steppingstone in his development, or, irrationally, I considered the possibility that he would forget me altogether. That time in isolation brought home for me the overwhelming love I felt for my family.
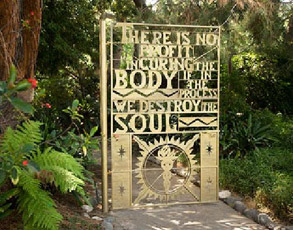
By nuking me to the bones and poisoning me near death, my care team was knocking me down just to build me up again. But isn’t that how it’s always been?
As babies begin to learn to walk, they fall down and get back up. After a failure at school, during work, in a relationship, don’t we pick ourselves up and return to it, wiser and more skilled than before? If we don’t get back up, we never have a chance to apply the knowledge we’ve gained. Without experiencing and understanding suffering, we cannot learn to move beyond it.
***
On Saturday, July 23, 2011, I wrote on my CaringBridge journal: For all who have donated blood products, thank you. For those considering donating, please know they will not go to waste. Yesterday, I received a bag of blood and a bag of platelets; today I received a bag of platelets. Tomorrow, who knows? But with your generous donations, I’ll have a better chance of receiving what I need when I need it. Thank you to all the donors, near and far!
***
Why are blood drives so commonplace? Because blood banks are chronically low on supply. When my leukemia was running rampant in my body in early 2011, the multiplying immature white blood cells were crowding out the red blood cells. I needed blood infusions, sometimes on a nearly weekly basis, to regain balance in my blood.
Later in the spring, when my white blood cell counts were very low from the rounds of chemotherapy, causing me to be neutropenic, or vulnerable to infection, I was often low on platelets in my blood. Low platelet counts can result in easy bruising or unstoppable bleeding. I received donated platelets almost every other day for weeks after my bone marrow transplant (BMT).
At my BMT time, people turned out for two blood drives in my California hometown on my behalf. Family, friends, and strangers all gave of themselves to help me during my time of need. The donations were in keeping with the precious town where I grew up and then returned to for comfort during my trials and tribulations with my leukemia diagnosis.
Giving of oneself, whether in the form of a blood product or through a kind word to a stranger, keeps us connected. In a world of isolating social media, real connections are more valuable today than ever. A handwritten letter, a handshake, a hug—how many have you received today? This week? This month? It’s more important to give someone a word of praise than a virtual thumbs-up. Sharing your gratitude up-close and personal with another person makes us human. And humanity needs the gift of giving to each other.
***
During my stints in the hospital, I surrounded myself with reminders of home, friends, and family, which brought smiles to my face while here at City of Hope. I taped up pictures of my guys from some of our jaunts last fall and winter, birthday cards, and ten flying cranes on a string created by Jonathan’s nephew, Evan. Jonathan hung up a special handmade quilt his friend, Carrie, made and my medal from finishing radiation as well as put up the black-and-white photo of Eliott and me on the outside of the door, so that everyone coming to visit me would see that picture of me hugging Eliott the night before I went into the Virginia hospital to start treatment for my Ph+ALL. Though it’s still a hospital room, I’ve made my mark on it.
***
That photograph of hugging baby Eliott, my twelve- month-old son, my weepy eyes closed to the camera, his thin arms wrapped around my neck, his beautiful face in profile, round cheek belaying a toothy grin, his eyes shining in the joy of the moment of a warm embrace. Eliott did not understand why his Mommy was crying that evening; he just knew I was hugging him, and he hugged back.
So many employees who worked on the Helford Hospital fourth, fifth, and six floors at City of Hope knew and remembered me because of that black-and-white moment in time captured by my husband. That special photograph told all who entered my hospital room that I had a precious bundle of joy to live for. The picture of love touched my care team and, I believe, made them work just a bit harder to keep me going, to propel me toward seeing my son again.
Those early days after BMT were a blur of nurses, aides, doctors, and my faithful companion by my side: my husband. I slept many hours of the day, mellowed out on pain medicine delivered via IV. Jonathan was there watching over my care, scrutinizing my daily patient reports for signs of engraftment, asking my care team the hard questions of what the daily blood draws were really saying about my progress. He never let up, which led to his having a few enemies as well as some admirers. His goal was to reunite our family, if only for a few minutes a day in the lobby of the sixth floor of Helford for a masked kiss and a joyful embrace.
***
By Monday, August 1, 2011, I wrote on CaringBridge this weekend, my numbers went way up. On Saturday, I went from 0.2 white blood cell count (WBC) to 0.3 WBC; on Sunday, from 0.3 to 0.5 WBC. So I’m now half way to seeing Eliott. But it’s not just about the numbers here at City of Hope. It’s about healing all parts of the patient: the mind, body, and spirit. I’ve had opportunities to work with rehabilitation therapists to get my arms and legs stronger. The recreation therapist helps keep my mind nimble with games and crafts. And the psychological therapist helps keep my spirits up.
***
During my weeks of isolation, members of my care team came to my room to tend to my emotional, mental, and physical states. Though I was often zonked out from fatigue or pain medicine, the team members were always kind and upbeat. These interactions broke the monotony and loneliness that built up between my husband’s bedside visits. I had always considered myself hermitlike, craving quiet time alone. My medical isolation changed that notion.
We humans are social creatures, built to gather together, whether it is to break bread or to sing or dance. To thrive, we need to talk with one another, to hold hands, and to hug each other.
When all that is taken away, it can be hard to remember how to embrace and even engage in a conversation. We lose a part of ourselves when isolated from others. I no longer crave that hermit life; instead, I rejoice in time with my family and friends.
***
By Sunday, August 7, 2011, I wrote that I already was feeling much better. I got to have a brunch social engagement with Eliott, at which he unpacked a picnic from a Trader Joe’s bag, which included a water bottle, an apple, a banana in a keeper, a box of breakfast bars, and some cogs that go with a toy. He placed the items on the coffee table, then asked for some apple by name, the first time I got to hear him say apple! I think he really enjoys being able to communicate his requests with words rather than pointing and grunting.
Though Eliott was going to town on the apple and occasionally nibbling on the banana, I’ve not been eating solid food for a while. But I might try something this afternoon. I’ll report back on how it goes.
***
At less than nineteen months, Eliott began to talk. I was alive to witness that milestone in his life.
It is amazing to recognize all of Eliott’s accomplishments during my six-week stay in the hospital for my BMT. He began to sort and organize objects, point to and request by name certain items, typically foods, and play with multipiece toys. Because of Dr. Stein’s special authorization that allowed me to visit with Eliott on the sixth- floor lobby, I got to watch my baby boy’s evolution.
Even through the lines connecting me to the IV pole heavily downloaded with medical apparatus as well as the mask covering most of my face, my little guy still recognized me as his Mommy. Eliott would sit on my lap to read short board books, and he would always give me a hug at the end of each visit.
I treasured our visits, especially after having been in isolation away from Eliott.
***
Today, Tuesday, August 9, 2011, was a solid day. Dr. Stein announced he would take away the pain pump completely. As I’m able to eat more and not have issues with vomiting, he will discontinue more of the IV medication, which I then will receive by mouth — about the same number, though different variety, of pills that I took when out and about before the BMT. I got to see my guys, which included reading a book to Eliott, and I was able to steal a hug from him while he was briefly sitting on my lap. He continues to evolve and grow in such magical ways. Jonathan and Joanna, through words and pictures, share many of these milestones when they first occur, then I often see them revealed a few days or weeks later during visits. I aim to be home before Eliott’s nineteen- month-old birthday, which is August 22. Jonathan was kind enough to return to the hospital to help me decide what to try to eat, reminding me that my stomach is still small and even a few bites of broth with white rice is a good thing. Had another small meal, and then took a shower, which means I’m off the IV pole for an hour. Time to rearrange the room, comfortably sit by the window, and go for a walk holding hands with my husband. The best part is always holding hands.
***
Whether it’s stealing a hug from an active toddler or holding hands with a partner, human contact is so important for everyone. Even through gloves and masks, that contact kept me going through the weeks in the hospital after my BMT.
There were times when everything seemed so surreal, what with the pain medication and procedures to keep me safe from infection, yet that human contact made all the difference. I remember one time when a nurse was changing the dressing on my PICC line—a once a week affair—and the alcohol scrub was so painful, with each stroke of the wand, I wanted to kick and scream, but I couldn’t move. Plus, the cramping of my rejuvenating digestive system was extremely painful—it hurt so badly I wanted to curl up in a ball, but I had to stay still for the nurse. I was disconnected from my pain pump (so that she could change the dressing), therefore I had no pain medication for comfort. Jonathan found heat packs for the cramping, and then he held my hand. Holding onto his hand so hard I’m sure I left bruises made the ordeal bearable.
Touch is so vital to our being, yet we take it for granted until it’s restricted through illness or other incapacitation. From the time we are born, we crave human contact. Babies cry out for nourishment, not only of the mother’s milk variety but also for the warm touch of a caress. I believe touch is a universal form of soothing for humans and animals alike. And touch can make the difference between surviving and dying.
***
Wednesday, August 10, 2011, day marks a full month, 31 days, in hospital. My hopes are high, based on a cryptic comment from Dr. Stein, that I might go home at the end of next week, which would be August 19. That timing would fulfill my wish to be home in time to celebrate Eliott’s nineteen-month-old milestone, which would be great! If it doesn’t happen, I won’t be too heartbroken.
***
By the time I left the Helford Hospital after my BMT, nearly six weeks had passed. When I first learned of my terminal diagnosis, I stayed in my Virginia hospital room for just about six weeks. I believe it was no coincidence that there were these timely bookends. My six or so weeks in the Virginia hospital, with its way of reducing my life like a Shrinky Dink, readied me for the BMT conditioning. Without my confinement in Virginia, I would not have been prepared for the isolation of the BMT time. And logging the weeks, days, hours, and minutes away from my loved ones once made it almost bearable a second time.
***
Thursday, August 18, 2011: I’ve been feeling well, and the doctor has been tapering me off IV medications, having me take more by mouth this week. Today, I was disconnected from my IV completely (though I still have the PICC line in my arm for blood draws). Everything is on track for my discharge from the hospital tomorrow, Friday. I’m very excited and a little nervous. Excited to be getting back home with my guys; nervous about how much of a burden I might be to my caregivers, especially being on a low-bacteria diet. The low- bac diet means no restaurant food, nothing raw except specially treated (bleached) bananas, apples, and oranges, and nothing heated in the microwave unless it comes out of a can. By all accounts, I’m eating well, just not much of things that might be hard on my new digestive system, such as dairy, which is tough on a veggie girl! Jonathan has reassured me that I will not be a burden, so I have to take his word for it. I can’t wait to be in a normal bed without people pestering me every few hours for blood or vitals or whatnot!
***
I didn’t write in my CaringBridge journal entry about how scared I was to leave the protective confines of the hospital. My mind whirled with what might go wrong. Perhaps I would eat some badly prepared food that would make me sick. Maybe I wouldn’t be able to keep down my medicines. What if someone in the house got sick—would I get the bug, too? How would Jonathan be able to juggle taking care of Eliott and me? Would I have time to participate in family affairs and still get enough rest? Who would check me for signs of infection such as fever? And, perhaps most gravely, would I end up with Graft Versus Host Disease (GVHD)?
When introducing, or grafting, stem cells into a patient, or host, there is typically some disagreement between the two, which leads to GVHD in the patient. Many doctors believe a certain level of GVHD is good because the newly introduced stem cells go after any remaining leukemic cells and rid the patient’s body of them. Too much GVHD, though, can be debilitating to the patient and even cause failure of vital organs such as the liver.
Somewhere around 85 percent of BMT patients end up with some form of GVHD. The disease usually can affect the digestive system, the skin, the lungs, the liver, or the eyes. Some unfortunates have multiple GVHD attacking more than one part of the body. There are two main types of GVHD: acute and chronic. Diagnosed within the first one hundred days of BMT, acute GVHD, most often of the digestive tract, can diminish and even resolve over time. Chronic GVHD stays with patients longer, often for the rest of their lives.
Would I end up with GVHD? And, if so, how bad would it be?
***
I so wanted to be one of the 15 percent of BMT patients who avoid all GVHD symptoms. But, alas, I was not. Ten days after I was released from the hospital—after just ten days of freedom—I returned to Helford Hospital at City of Hope. Unable to keep down my medications or much food and with rampant diarrhea, I trudged back into Helford, wondering if the hospital name was misspelled—why not name it a bit of Hell?
Though I was glum on my return, my care team nurses cheerfully called it a tune-up. They claimed it was completely normal to return for a visit not long after initial discharge. And, truthfully, it was better to find out sooner rather than later if I had some sort of GVHD.
My care team restricted me to a clear-liquid diet in anticipation of specialists performing tests. The doctors wanted to determine where my digestive tract was having trouble. Turns out I had a touch of GVHD in my gut. With a diagnosis, the doctors could prescribe medications to help with the symptoms.
After a couple of days, I felt well enough to go home. I left Helford with my head held high, recognizing that a touch of GVHD meant any last lurking leukemic cells would be caught up in the battle between my old self and the new engrafting immune system. I would have a better chance of outliving the cancer—and becoming a happy outlier—by suffering through some acute GVHD.
During the critical period of the first 100 days, patients are at their most vulnerable. Many end up with life-threatening infections, and some patients find out through bone marrow biopsies on Day +100 that the BMT was a failure. I wondered how many more times I would end up in the hospital during my first 100 days post-BMT.
***
I was discharged from the hospital yesterday Thursday afternoon, September 1, 2011. On some new medications, some which help with nausea, some which encourage appetite, some to work on the GVHD. All in all, I’m feeling OK and just trying to be sure not to overdo. Several City of Hope team members reminded me that my job right now is to eat well, relax, rest enough, and focus on healing. Knowing that I’m almost half way through the 100 days (in which the doctors look for infection and such the most) is encouraging, as are all your notes—thanks for your support!
***
Once home again, my focus was to eat a high-protein diet, kick my feet up, get lots of sleep, and put what energies I had toward healing. After more than seven months, I finally had a job again: to be a “recoverer,” as my therapist coined it.
***
In February 2011, Erin Michaela Sweeney was diagnosed with ALL. She is now a writer, mommy, yogini, daughter, editor, sister, and napper extraordinaire who lives in Claremont, California. This story is an adapted excerpt from her memoir, Every Breath Is a Gift: Reflections on My Leukemia Journey. For every book sold, it’s still good to be alive press will donate $1 profit to Be the Match. For more information, please go to www.ErinMichaelaSweeney.com or email to [email protected].
Originally published in The CLL Tribune Q4 2015.

















