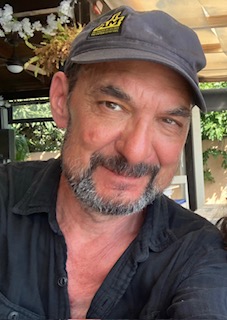
My friend Mark Silverstein passed away on September 12, 2024. After 13 years of living with CLL, his cancer transformed into Richter’s transformation (also called Richter’s syndrome), a more aggressive lymphoma that, despite some remarkable remissions, finally took his life.
For years, Mark led CLL Society’s support group in Toronto. As a psychotherapist specializing in palliative and hospice care, he used his own hard-fought wisdom and experience with CLL to help others with their cancer until his last days.
I was blessed to have many sweet and deep conversations with him over the last several months of his too-short life. I miss those calls.
During those conversations, I learned from him about balancing hope and realism. I learned about planning for the worst and the best at the same time. I learned from him about taking joy from tiny wins. I learned from him how to focus on what really matters in the end: family, friends, good work, and a life well lived.
I also learned from him about GRAVY.
Gravy
August 21, 1988
No other word will do. For that’s what it was. Gravy.
Gravy these past ten years.
Alive, sober, working, loving, and
loved by a good woman. Eleven years
ago, he was told he had six months to live
at the rate he was going. And he was going
nowhere but down. So, he changed his ways
somehow. He quit drinking! And the rest?
After that, it was all gravy, every minute
of it, up to and including when he was told about,
well, some things that were breaking down and
building up inside his head. “Don’t weep for me,”
he said to his friends. “I’m a lucky man.
I’ve had ten years longer than I or anyone
expected. Pure gravy. And don’t forget it.”
His widow Nelia shared this poem and, more memorably, this unfinished reflection on his Richter’s transformation diagnosis that follows below, cut short by his passing.
His obituary can be read in the Toronto Star. He lived a good life.
Stay strong, we are all in this together.
Brian Koffman
By: Mark Silverstein (unfinished)
The fact that I’m writing this article is a miracle for those who love me. I’ve learned that it’s not often that things turn around the way they have and that in this 13-year CLL journey, I consider myself very fortunate. I also learned that life could end on the couch, quietly, almost still, just holding hands, looking at each other with love, spiritual connection, and, of course, some anticipatory grief.
In November 2023, through our local hospice, as a registered psychotherapist I delivered my own psychotherapeutic group program for individuals with no treatment options left and in palliative care. I often commented to my wife that I suspected I’d be part of the group one day, but I didn’t realize how quickly that would come to be. On February 2nd of this year, after 3 weeks in the hospital, my hematologist came to us and, with a great deal of emotion, let us know that I had only 3-4 weeks to live. It turned out I had developed Richter’s Transformation, presenting as an 11cm mass wrapped around my heart. Between the effects of that and after one treatment of R-CHOP, I was too weak to endure a more intense and involved treatment such as epcoritamab (Dr. Koffman’s current treatment).
When I got home from the hospital, I was an absolute mess – lost over 20 lbs., was on oxygen 24×7, a Foley catheter and pee bag by my side, and I could barely walk due to de-conditioning from high dose steroids and chemo. I depended on my wife, family, and friends for almost everything. They were wonderful, most especially my wife, who helped me with almost everything as I lay there on the couch, unable to take care of myself. There was also a hospital bed delivered to the house and waiting for me, or what I began to refer to as my deathbed. But I never, not once, laid on that bed. Somehow, it felt like giving in to death. I decided that first night back home that I wanted to be in our bed, lying beside my wife, as that held a great deal of meaning as there was not a lot of time left. It was a struggle, and they (my wife and son) had to literally push me up those stairs, it almost felt like climbing a mountain every night but meaning drives us and gives us strength.
As I mentioned, it’s been 13 years and over eight treatments, including a stem cell transplant, and I was on pirtobrutinib when I entered the hospital this past January. My wife and I had, on many occasions, discussed that my aggressive version of CLL would eventually take me. After spending weeks in a hospital on multiple occasions, coming close to passing two other times, I was sure of one thing: I didn’t want to pass away there. In fact, on many occasions, we had talked at length about my coming home to die.
I’m not sure how to describe being told you have a few weeks to live. Of course, there was the initial disbelief, challenging my hematologist to do something the moment he told us, but acceptance came much quicker than I expected.
Throughout my years with CLL and as a psychotherapist working with a couple of hundred other cancer patients, I have helped people navigate their diagnosis both psychologically and emotionally. I have found, as a psychotherapist, that over the course of my disease, there have been moments where I said to myself – “I don’t know what it’s like.” Some of them I never will; having worked with many breast cancer patients, I will never know what it’s like as a woman to lose my breasts. And others I figured I would eventually know, like I don’t know what it’s like to be told I’m dying. Now I do!
The question was how I would react. Was I able to follow my own teachings to others, or was I, for lack of a better phrase, full of shit. In the palliative group program I created and ran called Journeys, there were a couple of main concepts – managing death anxiety, working to remain present to yourself and those around you, and finding meaning in the time you have left. The alternative was rolling up in a ball on the floor in fear of what was to come, preventing you from being present in whatever time you had left.
As a patient, I have found that understanding your disease, the treatment landscape, and being willing to advocate for yourself can be lifesaving. But there has been no other time that this was more true. I’m able to write this because my wife actually saved my life – she received an email from another health site, and the topic was Richter’s treatments. She could have buried it, figuring I was dying anyway, so what was the point? But instead, she reviewed it and made the choice to send it to me. This is where my understanding of things came into play – I noted zanubrutinib actually had a 15.4% complete response for Richter’s, and I assumed the partial response would be larger. Having been on ibrutinib as a second treatment in 2015, I knew the drug would be tolerable for my weak body. I also knew that, although I was resistant to a covalent BTK inhibitor, having just been part of the Loxo-305 clinical trial, pirtobrutinib could create a window where my mutational resistance would be minimized. Finally, I was able to communicate this to my hematologist and requested a “Hail Mary” as 15% was way better than zero. After almost 14 years, our relationship is as much of a partnership as anything else, and he bought into my request and began arranging for me to get the medication. When things like this happen, it’s hard not to believe the universe is somehow working in your favor. And it got even more clear when, a couple of days before I received the drug, I began to go downhill – I could feel the energy draining from my body, and my wife and son could see it too. They didn’t say anything to me but noted it between them. Then, that Friday morning, having our coffee in bed as we often do, I mentioned to my wife that I thought things were starting to go sideways. Literally, fifteen minutes later, the doorbell rang, and my new treatment (zanubrutinib) was delivered. Within a week, my health began to improve, and within a couple of weeks, my appetite started coming back. It’s been a long road back to feeling some sense of normality, but eventually, I shed the need for oxygen and the walker and did my physiotherapy work, where I can now walk and climb stairs myself. I even restarted my psychotherapy practice.
As I write this, I’m still on zanubrutinib, but expect that window to close soon, as we always understood it would only be a bridge to another treatment. Epcoritamab, the same treatment Brian Koffman is on, will be my next treatment and hopefully give me some more time on this earth. I would be remiss not to mention all the help, support, and guidance Brian has given me since this all began in January (as well as other times previous). I am grateful to call him a friend.
It has been a surreal process. One month, you expect to pass away, have prepared for it, and even have a service written for you. Then suddenly, you are living again. Going out with your wife for dinner and then to a music concert, something that she had expected to do alone to honor us. Except I was actually there. We still shake our heads about the fact I’m still alive; in fact, she calls me “dead man walking,” something meant and taken as a term of endearment. One of my favorite writers has a poem called “Gravy,” and that’s what it’s been so far all this extra time, it’s been all gravy.
I’ve always felt this, but dying has a way of clarifying things and getting rid of all the background noise. There is nothing more meaningful than the people we love and those who love us. So, I write this as a love letter to those people in my life, most especially my wife Nelia, who has cared for me, shared in my suffering, comforted me, and loved me through all this as well as all the previous years we have lived through my CLL.
Fear and regret have a way of keeping us from being in the present moment; either we are in the future or in the past, but either way unable to be where we actually are. Over the years, and I give credit to my psychotherapeutic training, I have learned to manage these things (especially fear) and have developed the ability to bring myself back to the present. I was told I was relapsing, and the very next day, I went to a client’s home who was passing away and was able to be present to the person’s suffering.

