Treating CLL is a little like a chess game. One needs to think a few moves ahead. Most treatments for CLL are not curative and when we do relapse, we better have a plan in place with some options that can knock back the leukemia again.
Fortunately, there are data that if a patient fails ibrutinib or other BTK inhibitors that they still have some good options with the best results coming from venetoclax, but there is also encouraging data for PI3K inhibitors such as idelalisib and duvelisib.
Dr. Anthony Mato who heads up the CLL program at Memorial Sloan Kettering in NY has published real world data to help guide us in how to sequence our increasingly powerful and complicated treatment options. Here is his research presented at ASH 2019: Optimal Sequencing of Ibrutinib, Idelalisib, and Venetoclax in CLL: Results from a Large Multi-Center Study of 683 US-Patients.
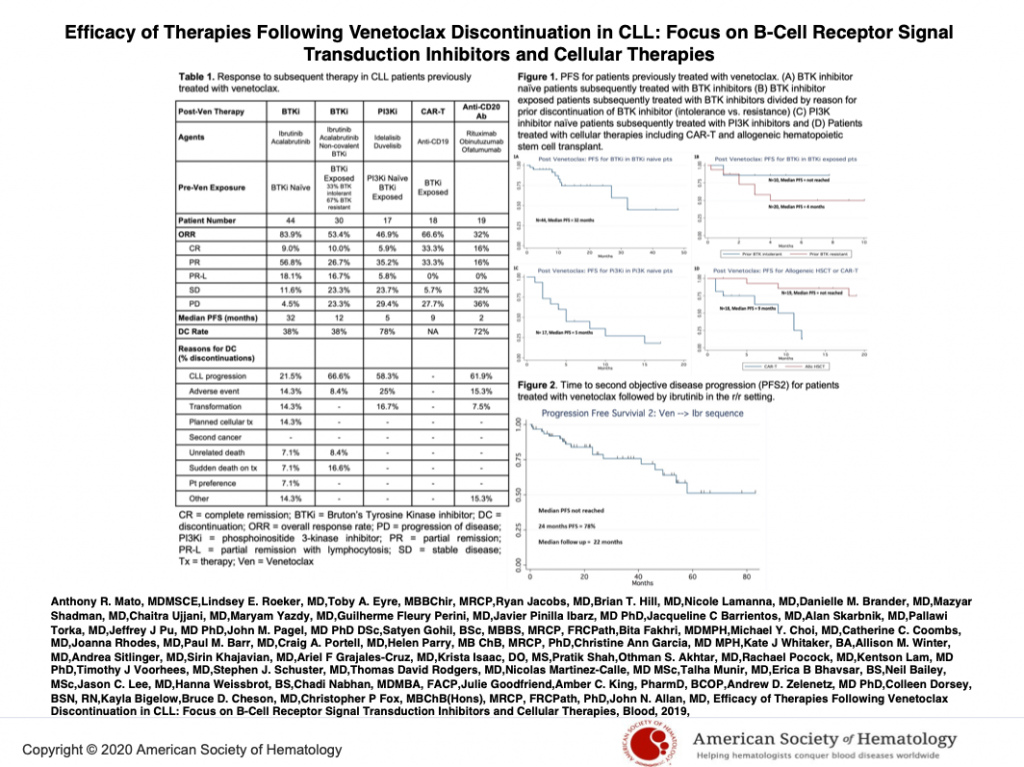
Now with the approval of venetoclax (ven) based treatments as a first line treatment for CLL, patients are rightly asking, what is my next step if I relapse after ven? What happens if I used venetoclax before I tried ibrutinib or acalabrutib? Will they work if and when I need them post ven?
As there have been only small numbers of such cases reported, Dr. Mato again assembled a team of top CLL researchers to try to answer these questions and see what was happening in the community.
At ASH 2019, in Orlando, FL, Dr. Mato discussed his findings that were presented as one of the oral CLL abstracts.
Takeaways
- Of the 267 patients studied, 62 had received venetoclax.
- 20 pts (32%) achieved a complete remission or CR and 14 pts (23%) achieved a partial remission or PR.
- There were 44 patients who received venetoclax but had never been treated with a BTK inhibitor such as ibrutinib or acalabrutinib.
- These were a difficult group to treat with venetoclax being on average the 4th line of therapy. We know it gets harder to control the disease with each relapse.
- About 80% responded to a BTK inhibitor after relapsing on venetoclax.
- Median progression free survival, or how long patients went without the disease progressing was 32 months. That’s pretty good.
- There is reason to believe results would be even better in patients who receive venetoclax sooner in the course of their CLL treatment and especially those who had this as their frontline therapy.
- There is also encouraging evidence that prior exposure to novel agents did not diminish the activity of cell-based therapies including CAR-T and hematopoietic stem cell (bone marrow) transplants.
- PI3K inhibitors such as idelalisib or duvelisib did see that about half the patients responded after failing ven, but the responses weren’t long lasting.
Conclusions:
As CLL is not curable for most patients with today’s therapies, short of a transplant and a few patients who do great with FCR, most of us will need multiple lines of therapy.
Today we have several great drugs to treat CLL, but how to combine them and how to sequence them is still a work in progress.
Dr. Mato offers us helpful data to begin to fill in some of the knowledge gaps, especially with his reassuring finding that there are good options after failing venetoclax.
My ASH 2019 interview with Dr. Mato can be viewed here:
This is the link to his oral abstract on this topic: Treatment Sequences and Outcomes of Patients with CLL Treated with Venetoclax and Other Novel Agents Post Introduction of Novel Therapies.
Here is some of the data from his presentation.
Stay strong.
We are all in this together.
Brian Koffman